By Ann Mikia
Nairobi, Kenya: The last International Aids Society Conference (IAS) held in Brisbane Australia ended with no ‘aha moment’. This is controversial depending on who says it. The proponents of the no aha moment felt there were no new scientific findings reported at the conference. Some people who have worked in the HIV and AIDS field either as reporters, trainers, or who have lived with the virus have a different opinion.
Professor Kenneth Ngure an expert on HIV and a lecturer at Jomo Kenyatta University of Agriculture and Technology (JKUAT) says there were a number of takeaways from the IAS Conference. What particularly stood out for him was the announcement of the Geneva patient who was the sixth person considered ‘cured’ of HIV.
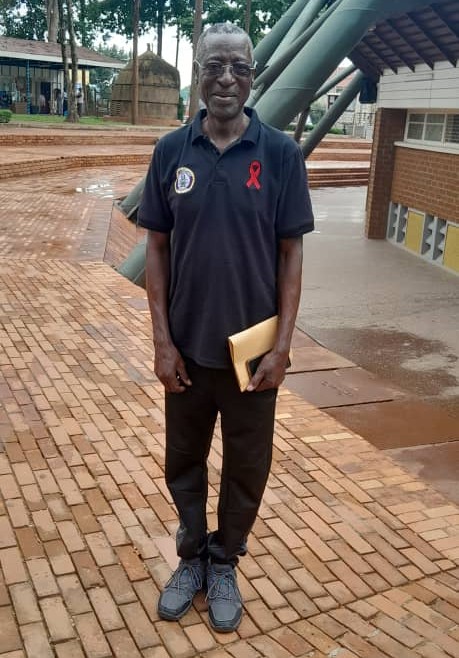
Dr. Stephen Watiti is a medical doctor in Uganda who has lived with HIV for thirty-five years. When he was diagnosed with the Human Immune Virus (HIV), there were no counseling services nor Antiretroviral therapy (ART) that prevented the virus from multiplying in the body. This left HIV patients to their devices on how to navigate their lives around the most feared incurable disease which killed many people, particularly in Sub-Saharan Africa.
In a regional webinar organized by the AIDS Vaccine Advocacy Coalition (AVAC), Dr. Watiti couldn’t hide his joy as he explained how the lives of people living with HIV have changed from the late 90s to date. He said the pill burden has reduced remarkably.
“I am on abacavir, lamivudine, and dolutegravir was taken as one tablet daily, which is okay with me, compared with nelifinavir which I took 3 tablets 3 times a day, didanosine one tablet daily, and one pill of stavudine, which I had to swallow back in 1999 when I started taking ARVs” he explains.
Australia stood out as a country that has reached epidemic control with very few HIV infections. What could Australia be doing that we are not? Professor Ngure says “First of all Australia reached their 90-90-90 target in 2020. This means testing 90% of people infected with HIV, putting 90% of those who test HIV positive on ART, and ensuring the viral load of 90% of those on ART is suppressed. They have also targeted the most at-risk population in HIV acquisition such as men who have sex with men and given them PrEP.”
Dr. Joshua Kimani, who is a clinical epidemiologist says it is possible to bring down the HIV infections.
“The first thing is to identify all the HIV-infected persons and put them on ARVs and if they agree to use the drugs the viral load will go down which is also referred to as U=U meaning Undetectable viral load is equal to Untrasmitable viruses and then anybody else who has unprotected sex with those infected can use Pre-Exposure Prophylaxis (PrEP) and the only thing we will be left to deal with are the sexually transmitted infections. That’s the only way to clear HIV in our setting” says Dr. Kimani.
According to the World Health Organization globally, almost three-quarters (71%) of people living with HIV in 2022 (76% of women and 67% of men living with HIV) have suppressed viral loads. Viral suppression enables people living with HIV to live long, healthy lives and to have zero risk of transmitting HIV sexually.
Great strides have been made in keeping HIV at bay. About forty years since the virus was detected in Kenya, there are a number of products that can be used ranging from female and male condoms, ARVs, the vaginal ring, Pre-exposure prophylaxis, and post-exposure prophylaxis. As Dr. Watiti confessed, combining the number of drugs to make the drug load bearable has also helped patients on the lifelong medication to adhere to treatment. What’s more, research is ongoing on a bi-monthly injectable ARV called carbotegravir. According to Dr. Watiti, “the injectable carbotegravir is on trial in Uganda only being administered on a few patients to get local evidence before being rolled out.” Professor Ngure says carbotegravir if approved by our government may be a game changer. Research shows that though injectable carbotegravir is not available in many countries, eight in ten women prefer long-acting injections to other products available.
Another challenge is that of ridding health-care facilities of stigma and discrimination along with removing laws and practices that make people, especially those from key populations, distrustful or fearful of health services. Early this year, Uganda’s president Yoweri Museveni signed into law the world’s harshest anti-lesbian, gay, bisexual, transgender, and queer (LGBTQ) bill which allows the death penalty for homosexual acts. This may make it difficult for people in gay relationships to access care freely.
Dr Watiti is against the law towards LGBTQ. He says “Most gay people are of course not openly gay, however, no one should be made to feel ashamed of how they practice their sex as long as it’s between two consenting adults in their right mind and within their private spaces. It’s however, a very populist legislation, with many people believing wazungu are using money to recruit, especially children into the practice. I personally believe no one should be left behind when it comes to prevention and treatment services but the current climate is quite toxic.”
For more Stories reach out to the writer through annmikia@gmail.com













